TP Threshold
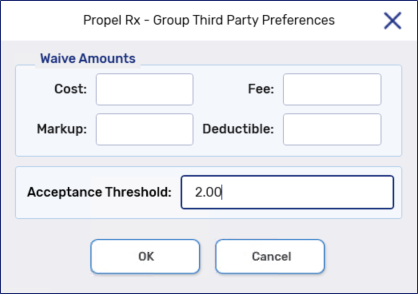
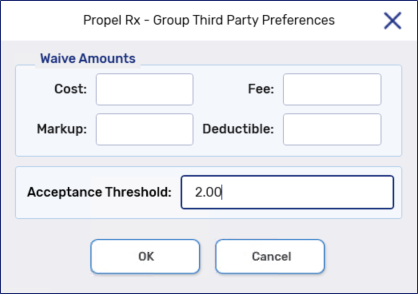
Group Third Party Preferences provide the ability to set group-specific waive and threshold amounts. This allows differences for Cost, Markup, Fee, and Deductible to be waived automatically based on the values entered in the corresponding waive fields. The Acceptance Threshold allows prescriptions to be accepted automatically without forcing the Claim Summary to be displayed.
Group Third Party Preferences provide the ability to set group-specific waive and threshold amounts that override the pharmacy-level Third Party Preferences. This allows differences for Cost, Markup, Fee, and Deductible to be waived automatically if the differences are less than or equal to the values entered in the corresponding waive fields. The Acceptance Threshold allows prescriptions to be accepted automatically without forcing the Claim Summary to be displayed.
Waives set in the Patient Folder Third Party tab apply regardless if the difference returned is greater than the waive amount.
When a Nursing Charge plan is part of the billing code for a prescription, the waive amounts and the acceptance threshold will be applied before the prescription is submitted to the Nursing Charge plan for payment. This allows differences to be waived or accepted before claims are billed to Nursing Charge. If a Nursing Charge plan is not part of the billing code, the waive amounts and the acceptance threshold will be applied before the prescription is submitted to Cash.
Differences are NOT waived by Propel Rx if the claim is NOT the last Third Party before the Nursing Charge plan in a co-ordination of benefits. Any differences will be sent to the next Third Party for payment. Only differences from the final Third Party in the co-ordination of benefits process will be waived. The same logic applies to the Acceptance Threshold; only differences from the final Third Party in the co-ordination of benefits process will be automatically accepted.
Use the dropdowns to learn more.
 Cost
Cost
This is the maximum value that will be waived automatically if a cost difference is sent back from the Third Parties that adjudicated the prescription.
This is the maximum value that will be waived automatically if a cost difference is sent back from the Third Parties that adjudicated the prescription. If the cost difference is greater than the value entered in this field, the waive is not applied.
 Markup
Markup
This is the maximum value that will be waived automatically if a markup difference is sent back from the Third Parties that adjudicated the prescription.
This is the maximum value that will be waived automatically if a markup difference is sent back from the Third Parties that adjudicated the prescription. If the markup difference is greater than the value entered in this field, the waive is not applied.
 Fee
Fee
This is the maximum value that will be waived automatically if a fee difference is sent back from the Third Parties that adjudicated the prescription.
This is the maximum value that will be waived automatically if a fee difference is sent back from the Third Parties that adjudicated the prescription. If the fee difference is greater than the value entered in this field, the waive is not applied.
 Deductible
Deductible
This is the maximum value that will be waived automatically if a deductible is sent back from the Third Parties that adjudicated the prescription.
This is the maximum value that will be waived automatically if a deductible is sent back from the Third Parties that adjudicated the prescription. If the deductible difference is greater than the value entered in this field, the waive is not applied.
For example, the deductible waive is set to $2.00. A Batch is run, and a deductible of $6.11 is returned for a prescription. The $2.00 waive is not applied to the prescription because the deductible returned exceeds the deductible waive entered for the Group. Conversely, if a deductible of $2.00 is returned, the waive is applied and the prescription cost is reduced to $0.00.
 Acceptance Threshold
Acceptance Threshold
This is the maximum value that will be automatically charged to patients without forcing the Claim Summary to be viewed. This applies to the sum of any differences and deductibles that are sent back from Third Parties that adjudicated the prescription. Therefore, if the sum of all these amounts is less than or equal to the value set as the Acceptance Threshold, the Claim Summary will not be displayed and the amount will be charged to the patient.